A New Minimally Invasive Procedure for Muscle, Back,
Neck Pain and Radiculopathy – The Myofascial Nerve
Block
http://www.anncaserep.com/open-access/a-new-minimally-invasive-procedure-for-muscle-back-neck-pain-9004.pdf
Omoigui S., Fadare A.
Abstract
This is the first description of a procedure targeting the myofascial tissues since Janet Travell’s
description of myofascial trigger points in 1942. However unlike trigger point injections, this
minimally invasive myofascial nerve injection is performed differently and targets the myofascial
tissues, peripheral innervations, posterior spinal structures and spinal nerve roots at the same
time. It is different from a trigger point injection that aims to block trigger points within a muscle.
Prolonged standing or sitting, posture and other multiple factors can create recurrent injuries
with attendant inflammation and episodically aggravate pain. Thus there is a need for a simple
intervention technique that can be performed from the medical clinic to the battlefield to quickly
relieve inflammation and prevent chronic pain.
Introduction
This myofascial nerve injection is also the first procedure for spine pain since epidural pain
injection was first described by Jean-Anasthase Sicard in Paris on April 20th, 1901 [1,2]. However,
at about the same time, Fernand Cathelin also from Paris had been treating patients with epidural
injections for some months already [3].
Incidentally, a few months after we published our novel short needle technique for paraspinal
muscle block in February 2016 [4,5], the Erector Spinae (ESP) nerve block was described in a
publication in September 2016, as a regional block for thoracic neuropathic pain [6-8]. The injection
is performed by a single shot or with a catheter insertion for continuous infusion (5 ml to 14 ml per
hour) [9,10]. The primary mechanism is thought to be a direct effect of local anesthetic via physical
spread and diffusion to the erector spinae muscles as well as neural structures in the fascial plane
deep to the erector spinae muscles and adjacent tissue compartments [11]. Satisfactory results have
been obtained in the treatment of both acute pain and chronic pain, and in some cases the ESP has
replaced the use of epidural injections.
Clear solution of medication injected under pressure from a 30 G 5/8 inch (15.6 mm) needles
travel a distance of 4 cm to 6 cm. As described in Sota Omoigui Short Needle Technique [4], utilizing
the physics principle of the law of conservation of mass, the increased velocity of the injectate is
sufficient to traverse the erector spinae muscles to the vertebral lamina and block the posterior
spinal structures and nerves at the level injected [4]. Compressing the soft tissue with one hand, and
injecting 1 ml to 2 ml Lidocaine 2% at the two most painful levels on each side of the vertebra or
spinous process, we have been able to achieve 60% to 100% of relief of axial and radicular pain within
5 min. Total dosage of Lidocaine must be below the toxic dose of 3 mg/kg without epinephrine.
Due to the small size and length of the needle, this technique can be performed not just by
pain specialist but by a primary care physician, physician assistant, nurse practitioner or any
medical service provider trained to do intramuscular injections. This myofascial nerve block can be
performed with or without imaging guidance in a variety of settings from the operating room to the
medical clinic to the battlefield.
This myofascial nerve block may be used in combination with an anti-inflammatory regimen,
including oral, IV or IM Steroid, Ketorolac/Diclofenac, Opioids, Ketamine, Ketorolac, Magnesium
Sulfate, Kineret, CGRP Blockers, Botulinum Toxin etc. These block or inhibit various inflammatory
mediators including prostaglandins (steroid, ketorolac/diclofenac), IL-1 Beta (Kineret) NMDA
receptors (magnesium sulfate, ketamine), Substance P (Botulinum Toxin) etc [12].
Omoigui S* and Fadare A
Department of Inflammation and Pain Research, LA Pain Clinic, USA
OPEN ACCESS
*Correspondence:
Sota Omoigui, Department of
Inflammation and Pain Research, L.A.
Pain Clinic, 4019 W. Rosecrans Ave,
Hawthorne, California, 90250, USA, Tel:
+1-310-675-9121; Fax: +1-310-675-
7989;
E-mail: medicinechief@aol.com
Received Date: 30 Apr 2022
Accepted Date: 18 Jun 2022
Published Date: 24 Jun 2022
Citation:
Omoigui S and Fadare A.
A New
Minimally Invasive Procedure for
Muscle, Back, Neck Pain and
Radiculopathy – The Myofascial Nerve
Block. Ann Clin Case Rep. 2022; 7:
2233.
ISSN: 2474-1655
Copyright © 2022 Omoigui S. This is
an open access article distributed under
the Creative Commons Attribution
License, which permits unrestricted
use, distribution, and reproduction in
any medium, provided the original work
is properly cited.
2
Omoigui S, et al., Annals of Clinical Case Reports – General Medicine
Remedy Publications LLC., | http://anncaserep.com/ 2022 | Volume 7 | Article 2233
Low back and neck pain causes more disability than any other
and accounts for the third highest health care spending after diabetes
and ischemic heart disease [13].
Subsequent to tissue injury, the initial immune reaction
generates an inflammatory milieu of chemical mediators that include
prostaglandin, interleukin 1-alpha, interleukin 1-beta, interleukin-4,
Interleukin-6 and interleukin-8 nitric oxide, tumor necrosis factor
alpha, histamine and serotonin [14,15].
Following this injury, there is increased nerve traffic in the sensory
neurons that travel to the spinal cord and stimulate the release of
inflammatory protein Substance P. The presence of Substance P and
other inflammatory proteins such as Calcitonin Gene-Related Peptide
(CGRP) neurokinin A and vasoactive intestinal peptide removes
magnesium induced inhibition and enables excitatory inflammatory
proteins such as glutamate and aspartate to activate specialized spinal
cord NMDA receptors and increase magnification of the nerve traffic
and pain stimuli.
Axial and radicular back pain is symptoms of injury that result in
a cascade of inflammatory mediators. Local anesthetic agents stabilize
nerve membrane and decrease pain by reducing the rate of discharge
of sensory nerve fibers and decreasing neurogenic inflammation [16].
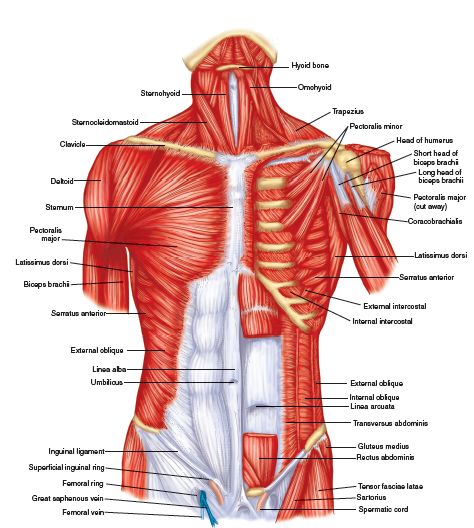
Current procedural injections for back, neck and radicular pain
focus on structures that are visible with imaging, skeletal system
(bones, joints, intervertebral discs) and central nervous system (brain
and spinal cord) components while completely ignoring the largest
organ in the spine and most often the initial site of injury, which
are the paraspinal muscles–cervical, thoracic and lumbar. The most
common pain procedures are essentially blind techniques as pain
triggers are targeted based upon structural pathology. Unfortunately
there is poor correlation between structural pathology and the
presence of back [17,18] or neck pain [19].
Myofascial tissues constitute a pain generator that is not
addressed in current interventional pain procedures. Randomized
controlled studies of current procedures have yielded conflicting
results. In a study by Dilke et al., [20] patients who received epidural
corticosteroids experienced less pain than controls, needed surgery
less often and returned back to work sooner. However and on the
contrary, Snoek et al., [21] showed that epidural steroid injection
was no more effective than a placebo injection in relieving chronic
symptoms due to lumbar disc herniation. In 2008, Staal et al. [22]
reported on a systematic review of the literature conducted with a
focus on randomized, controlled trials. Based on their analyses, the
authors made the conclusion that there is moderate evidence that
epidural corticosteroid injections are no more effective than placebo
injections for pain relief.
Other procedures range from transforaminal injections,
radiofrequency thermal lesioning of the medial branch nerves,
radiofrequency cryolesioning of the medial branch nerves, intradiscal
electrothermy (thermal burn to the intervertebral disc), and spinal cord
stimulation. Recent randomized control trials have also questioned
the effectiveness of these more invasive procedures. A multicenter,
randomized, double-blind, sham treatment controlled trial was
performed to determine the efficacy of radiofrequency lumbar facet
joint denervation. In both groups, there was significant improvement
in the Visual Analog Scale (VAS) [23]. In the Mint study, three
randomized clinical trials were conducted on the effectiveness of
minimal interventional treatments for participants with chronic low
back pain. Radiofrequency denervation combined with a standardized
exercise program resulted in either no improvement or no clinically
important improvement in chronic low back pain compared with a
standardized exercise program alone. In another randomized control
trial, assessing the efficacy of Radiofrequency (RF) denervation of the
cervical facet joints in chronic cervical facet joint pain the authors
stated that they did not observe significant differences between RF
denervation combined with injection of local anesthesia compared
with local anesthesia at 6 months follow-up. The need for pain
medication did not differ significantly between groups [24]. In another
randomized controlled trial, in patients with cervicogenic headache
the authors did not find evidence that radiofrequency treatment of
cervical facet joints was a better treatment than the infiltration of the
greater occipital nerve [25].
In one study the author stated that the evidence is poor for
cervical transforaminal epidural injections. Complications with
cervical interlaminar epidural injections are rare, but more commonly
occur with transforaminal epidural injections. These can be fatal and
include vertebral artery injury, systemic allergic reactions to radio
contrast agents, transient cortical blindness and brain injury [26],
stroke, paraplegia, quadriplegia, spinal cord and cerebella infarction
[27,28].
These trials raise the issue of questionable benefits, compared to
simpler procedures such as our myofascial nerve blockade.
As stated in the NIH, HEAL Initiative Fund Opportunity [29],
the field of musculoskeletal pain has largely focused on the skeletal
system (bones, joints, intervertebral discs) and central nervous system
(brain and spinal cord) components. The contribution of myofascial
tissues, especially fascia, and the interactions of fascia, muscles, and
peripheral nerves are understudied and remain mostly unknown. Pain
originating from muscles and fascia is likely an important component
of many severe and chronic pain conditions. The perimuscular fascia
is richly innervated with small-diameter fibers whose receptive fields
increase in the presence of inflammation. Thus myofascial tissues
play a significant role as pain generators.
The NIH noted that for many years, structural imaging was the
main tool to guide treatment decisions, including surgery. Meanwhile,
imaging and other objective measurements of “soft” tissues including
muscles, and connective tissues or “fasciae,” were not even considered
as musculoskeletal pain biomarker candidates. Thus NIH has called
for development of biomarkers of myofascial tissues for effective pain
management regimens.
In the last seven years, we have replaced epidural and facet joint/
nerve injections with a myofascial nerve block. We routinely perform
myofascial nerve injections, with or without ultrasound guidance to
relieve pain. We had observed during spinal procedures that a clear
solution of Lidocaine 2%, injected from a 30G 5/8 inch (15.6 mm)
needle, using a 3 ml syringe, and inserted just lateral to the spinous
process, into the paraspinal muscles, traveled a distance of 4cm to
6 cm [4]. This distance was sufficient to travel through the erector
spinae muscles down to the vertebral lamina and posterior spinal
structures and within minutes produce anesthetic block to relieve
radicular pain from the nerve roots [4].
In the last two years, the advent of erector spinae plane blocks that
are essentially myofascial blocks but utilizing longer needles inserted
to the target point, with large volumes of dilute local anesthetic has
validated our original but simpler myofascial nerve block (Figures 1-6
3
Omoigui S, et al., Annals of Clinical Case Reports – General Medicine
Remedy Publications LLC., | http://anncaserep.com/ 2022 | Volume 7 | Article 2233
and Video 1).
Discussion
When a 30 gauge needle is attached to a 3 ml syringe, the distance
of travel of medication from the syringe and needle into tissue will be
greater, because there is increased velocity through the smaller needle
and hence greater penetration of medication into the tissues.
Utilizing the equation of continuity, we can analyze what happens
to the fluid if the size of the tubing through which it flows, changes.
Figure 7 shows the pipe constricting from area A1
to area A2
. Since no
fluid can leave through the walls, the mass crossing each section of the
tube per unit time must be the same. Therefore the velocity of fluid
through the smaller area is faster than the velocity of the fluid through
the larger area. This phenomenon can be explained and quantified by
examining the flow rate of mass through the tubing. The equation of
continuity states that, in any steady state process, the rate at which
mass enters a system is equal to the rate at which mass leaves the
system:
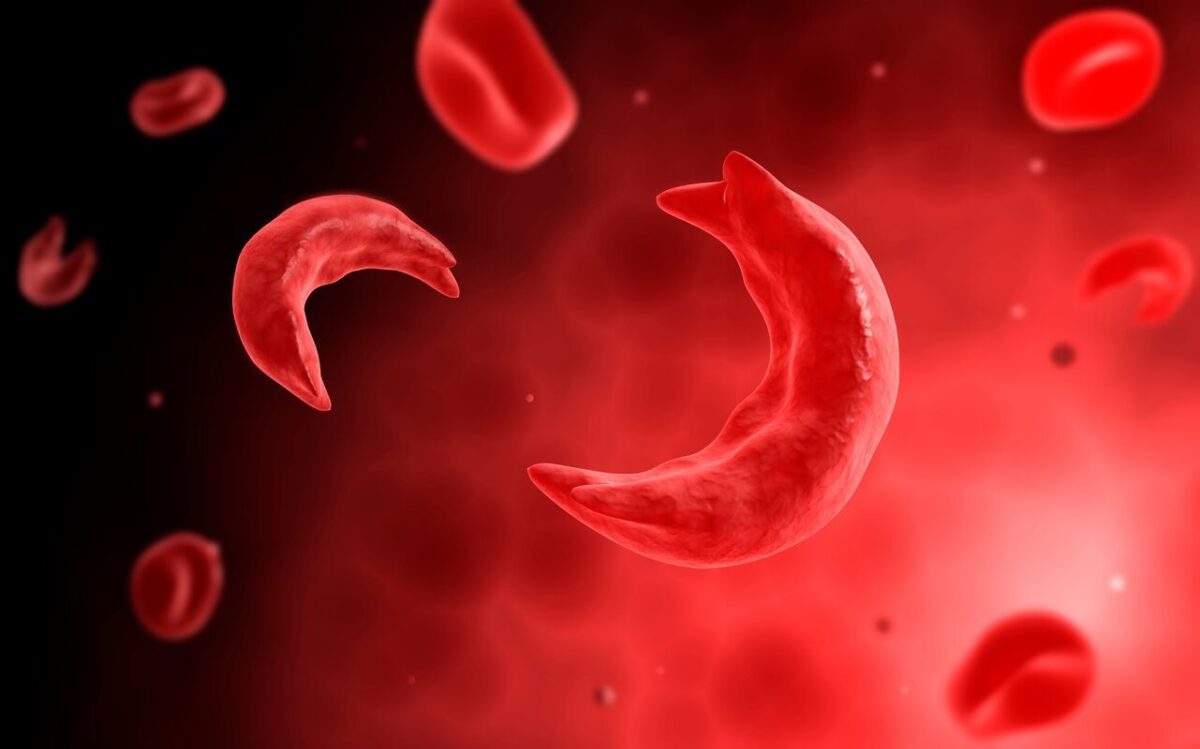
Figure 1: Comparison of a 30 G needle with an epidural and spinal needle.
Figure 2: Ultrasound screen showing the depth reached by medication
in tissue using a 30 G needle during a trigger point injection of the lumbar
paraspinal muscle.
From the screen of the ultrasound, the medication travels 4 cm to 6 cm (40
mm to 60 mm) into the muscle.
Figure 3: Myofascial Injection technique with ultrasound guidance. (SP:
Spinous Process).
Figure 4: Myofascial Injection technique-Showing 5/8 in length of the 30G
needle.
Figure 5: Myofascial Injection technique, without ultrasound guidance.
Figure 6: Myofascial Injection technique, needle halfway inserted.
4
Omoigui S, et al., Annals of Clinical Case Reports – General Medicine
Remedy Publications LLC., | http://anncaserep.com/ 2022 | Volume 7 | Article 2233
Flow rate through A1
= Flow rate through A2
d1
A1
v1
= d2
A2
v2
Therefore,
dAv = Constant
This equation expresses the law of conservation of mass in fluid
dynamics.
If fluid is incompressible, then the density is constant (d1
= d2
),
Then,
A1
v1
=A2
v2
Where
A1=Area in tube 1
v1=Velocity in tube 1
A2=Area in tube 2
v2=Velocity in tube 2
d=density of the fluid
For our purpose, A1v1 will be a syringe and A2v2 the hypodermic
needle. When a higher gauge (smaller) needle is used, with a 3 ml
syringe, the distance of travel of medication from the syringe and
needle into tissue will be greater, because there is increased velocity
through the smaller needle and hence greater penetration of
medication into the tissues.
Advantages
Clear fluid medications can be injected to traverse and provide
a therapeutic effect at a distance to the needle point e.g. paraspinal
muscles and lamina.
Limitations
This targeted structure must be within 6 cm distance and not
obstructed by bone e.g. a hip or knee joint.
Myofascial Injection Technique
With the Myofascial Injection Technique for Spinal Pain, the
spine is palpated to locate the most painful sites. A short 30G 5/8
inch needle is inserted adjacent to the spinal process or vertebra at
the level of those sites. The soft tissue is compressed and the needle
is advanced just past the subcutaneous tissue into the muscle layer,
and 1 ml to 2 ml of local anesthetic solution (preferably 2% Lidocaine
for most sites) is injected in each site. If performed under ultrasound
guidance the solution will be seen to spread 4 cm to 6 cm deep into
the paraspinal muscle, down to the lamina and posterior spinal
structures. The injection is repeated at the 2 to 4 most painful sites,
keeping in mind not to exceed the toxic dose of the local anesthetic
(3 mg/kg). The number of sites injected is limited by the volume and
concentration of local anesthetic injected so as not to exceed the toxic
dose of anesthetic.
With the myofascial injection, the soft tissue is compressed and the
needle is inserted close to its hub (5/8 in), the medication is injected to
reach the target site. In most instances, it is no longer necessary to use
longer and bigger gauge needles for epidural injections for treatment
of axial pain and radiculopathy. With a myofascial injection, the
medication can be pushed under pressure through the erector spinae
muscle to block the posterior spinal structures, using a smaller shorter
needle. Use of such a short small bore needle such as the BD 30G
5/8 inch needle will make myofascial injections much safer as there
is significantly decreased risk of needle trauma. This technique is also
useful in patients who are anti-coagulated. Compression of the skin
and subcutaneous fatty tissue reduces the distance of travel required
for the medication to penetrate through the paraspinal muscle to the
posterior spinal structures.
Distances
Clear solution of medication injected under pressure from a 30G
5/8 inch (15.6 mm) needles travel a distance of 4 cm to 6 cm.
In the lumbar spine, the distance from the skin to the ligamentum
flavum is 3 cm to 8 cm [30-32]. In the upper thoracic spine the distance
from skin to the lamina with a paramedian approach, 1 cm from the
midline, is 4.2 cm, middle thoracic spine is 3.7 cm, lower thoracic
spine is 3.6 cm and lumbar spine is 4.0 cm. The average distance from
skin to the epidural space with a paramedian approach, 1 cm from the
midline, in the upper thoracic spine is 5.6 cm, middle thoracic spine is
5.2 cm, lower thoracic spine is 4.4 cm and lumbar spine is 4.7 cm [33].
The mean distance from the skin to the transverse processes and facet
joint articular processes, ranges from 3.2 cm to 5 cm, as measured in a
study utilizing a 3 MHz to 5 MHz ultrasound probe see Figure 8 [34].
We have had a variable duration of pain relief from one week to
one year and similar to the epidural steroid and facet nerve injections
Figure 7: The pipe constricting from area A1 to area A2.
Figure 8: Mean distances (mm) between skin and transverse processes
(TPR &TPL) and skin and articular processes (APR & APL) by vertebral level
(TPR: skin to transverse process at the right side, TPL: skin to transverse
process at the left side, APR: skin to articular process at the right side. APL:
skin to articular process at the left side).
It can therefore be seen that by compressing the soft tissue and shortening
the distance, with our technique for procedural injections utilizing a short
small bore needle such as the BD 30G 5/8 inch needle, medication can be
delivered at a distance, under pressure, to travel to block pain generators
including peripheral nerves in the muscle, fascia, as well as in the posterior
spinal structures in including the medial branch nerves, facet joints and
lumbar nerve roots. This is the first procedural technique that can block
multiple pain generators in just one injection.
5
Omoigui S, et al., Annals of Clinical Case Reports – General Medicine
Remedy Publications LLC., | http://anncaserep.com/ 2022 | Volume 7 | Article 2233
that we previously performed. There have been no complications with
this technique, in more than 500 procedures.
Conclusion
The Myofascial nerve injection is a simple intervention technique
that can be performed from the medical clinic to the battlefield to
quickly relieve inflammation, treat acute pain and prevent chronic
pain.
It is the first procedure that targets the myofascial tissues,
peripheral innervations, posterior spinal structures and spinal nerve
roots at the same time.
Due to the small size and length of the needle, this technique
can be performed not just by pain specialist but by a primary care
physician, physician assistant, nurse practitioner or any medical
service provider trained to do intramuscular injections.
The therapeutic and anti-inflammatory effect of the myofascial
nerve injection is from the neuro-modulatory activity local anesthetic
(preferably 2% Lidocaine for most injection sites). The myofascial
injection procedure using the Sota Omoigui Short Needle Technique
may be combined with an anti-inflammatory regimen that may be
administered by the parenteral route.
Video 1: Video of ultrasound during myofascial injection
procedure.
References
1. Ter Meulen BC, Weinstein H, Ostelo R, Koehler PJ. The epidural treatment
of sciatica: Its origin and evolution. Eur Neurol. 2016;75(1-2):58-64.
2. Sicard MA. Les injections médicamenteuses extradurales par voie
sacrococcygienne. C R Seances Soc Biol Fil. 1901;53:396.
3. Cathelin F. Une nouvelle voie d’injection rachidienne: Méthode des
injections épidurales par le procédé du canal sacre – applications à
l’homme. Compt Rend Soc de Biol. 1901.
4. Omoigui S, Ogbeiche C, Fadare A. Reinventing IM and procedural
injections: The Sota Omoigui short needle technique. Practical Pain
Management. 2016:28-34.
5. Omoigui S. Merging physics with anesthesia presented at the International
Anesthesia Research Society Conference, May 16th, 2019, Montreal,
Quebec, Canada.
6. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae
plane block: A novel analgesic technique in thoracic neuropathic pain. Reg
Anesth Pain Med. 2016;41(5):621-7.
7. Ueshima H, Hiroshi O. Spread of local anesthetic solution in the erector
spinae plane block. J Clin Anesth. 2018;45:23.
8. Ivanusic J, Konishi Y, Barrington MJ. A cadaveric study investigating the
mechanism of action of erector spinae blockade. Reg Anesth Pain Med.
2018;43(6):567-71.
9. Tsui BC, Mohler D, Caruso TJ, Horn JL. Cervical erector spinae plane
block catheter using a thoracic approach: An alternative to brachial plexus
blockade for forequarter amputation. Can J Anaesth. 2019;66(1):119-20.
10. Jadon A, Jain P, Sinha N. The erector spinae plane block for postoperative
analgesia in abdominoplasty – A case report. BAOJ Anesthesia.
2017;1(1):001.
11. Chin KJ, El-Boghdadly K. Mechanisms of action of the Erector Spinae
Plane (ESP) block: A narrative review. Can J Anaesth. 2021;68(3):387-408.
12. Omoigui S. The biochemical origin of pain: How a new law and new drugs
have led to a medical breakthrough in the treatment of persistent pain.
State of the Art Technology Publishers. 2002.
13. Dieleman JL, Baral R, Birger M, Bui AL, Bulchis A, Chapin A, et al. US
spending on personal health care and public health, 1996-2013. JAMA.
2016;316(24):2627-46.
14. Omoigui S. The biochemical origin of pain–proposing a new law of pain:
The origin of all pain is inflammation and the inflammatory response. Part
1 of 3–a unifying law of pain. Med Hypotheses. 2007;69(1):70-82.
15. Omoigui S. The biochemical origin of pain: The origin of all pain is
inflammation and the inflammatory response. Part 2 of 3-inflammatory
profile of pain syndromes. Med Hypotheses. 2007;69(6):1169-78.
16. Waxman SG. The molecular pathophysiology of pain: Abnormal expression
of sodium channel genes and its contributions to hyperexcitability in
primary sensory neurons. Pain. 1999;6:S133-S140.
17. Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal
magnetic-resonance scans of the lumbar spine in asymptomatic subjects.
A prospective investigation. J Bone Joint Surg Am. 1990;72(3):403-8.
18. Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian
D, Ross JS. Magnetic resonance imaging of the lumbar spine in people
without back pain. N Engl J Med. 1994;331(2):69-73.
19. Van der Donk J, Schouten JS, Passchier J, van Romunde LK, Valkenburg
HA. The associations of neck pain with radiological abnormalities of the
cervical spine and personality traits in a general population. J Rheumatol.
1991;18(12):1884-9.
20. Dilke TF, Burry HC, Grahame R. Extradural corticosteroid injection
in management of lumbar nerve root compression. Br Med J.
1973;2(5867):635-7.
21. Snoek W, Weber H, Jorgensen B. Double blind evaluation of extradural
methyl prednisolone for herniated lumbar discs. Acta Orthop Scand.
1977;48(6):635-41.
22. Staal JB, de BR, de Vet HC, Hildebrandt J, Nelemans P. Injection therapy
for subacute and chronic low‐back pain. Cochrane Database Syst Rev.
2008;2008(3):CD001824.
23. Van Wijk RM, Geurts JW, Wynne HJ, Hammink E, Buskens E, Lousberg
R, et al. Radiofrequency denervation of lumbar facet joints in the treatment
of chronic low back pain: A randomized, double-blind, sham lesioncontrolled trial. Clin J Pain. 2005;21(4):335-44.
24. van Eerd M, de Meij N, Kessels A, Patijn J, Weber W, Wintraecken V,
et al. Efficacy and long-term effect of radiofrequency denervation in
patients with clinically diagnosed cervical facet joint pain: A double-blind
randomized controlled trial. Spine (Phila Pa 1976). 2021;46(5):285-93.
25. Haspeslagh SR, Van Suijlekom HA, Lamé IE, Kessels AG, van Kleef M,
Weber WE. Randomised controlled trial of cervical radiofrequency lesions
as a treatment for cervicogenic headache [ISRCTN07444684]. BMC
Anesthesiol. 2006;6:1.
26. McMillan MR, Crumpton C. Cortical blindness and neurologic injury
complicating cervical transforaminal injection for cervical radiculopathy.
Anesthesiology. 2003;99(2):509-11.
27. Tiso RL, Cutler T, Catania JA, Whalen K. Adverse central nervous system
sequelae after selective transforaminal block: The role of corticosteroids.
Spine J. 2004;4(4):468-74.
28. Manchikanti L, Falco FJ, Diwan S, Hirsch JA, Smith HS. Cervical radicular
pain: The role of interlaminar and transforaminal epidural injections. Curr
Pain Headache Rep. 2014;18(1):389.
29. NIH Heal Initiative. Department of Health and Human Services.
30. Joseph P. Geophysical fluid dynamics. Springer. 1987:10-3.
31. Bloomfield, Louis. How Things Work: The physics of everyday life. 3rd Ed.
John Wiley and Sons; 2006. p. 153. ISBN 0-471-46886-X.
6
Omoigui S, et al., Annals of Clinical Case Reports – General Medicine
Remedy Publications LLC., | http://anncaserep.com/ 2022 | Volume 7 | Article 2233
32. Neuraxial Blockade Anatomy and Landmarks.
33. Ogura A, Inoue T, Wajima Z, Yoshikawa T, Imanaga K. Skin to vertebral
lamina distance as a principal landmark for the epidural puncture using
the paramedian approach. Eur J Anaesthesiol. 2000;17:96.
34. Gharaei H, Imani F, Solaymani-Dodaran M. Survey of sonoanatomic
distances for lumbar medial branch nerve blocks in healthy volunteers.
Korean J Pain. 2014;27(2):133-8.